AnalyticsBreaking News
Breast Cancer Screening, writes Dr. Lopamudra Das Roy


August 10: Over the years, Breast cancer has been afflicting and engulfing our society. Breast cancer is the top cancer in women both in the developed and the developing world. About 1 in 8 U.S. women will develop invasive
breast cancer over the course of her lifetime. Breast cancer frequency is also increasing rapidly in developing countries where most cases are diagnosed in late stages.
Detecting Breast Cancer Earlier can save lives by Breast screening processes:
Mammogram: The most recent American Cancer Society guidelines recommend women aged 40 to 44 should have the choice to start annual Breast cancer screening with mammograms (x-rays of the breast), if they wish to do so. Women age 45 to 54 should get mammograms every year. Women 55 and older should switch to mammograms every 2 years or can continue yearly screening. All women should be familiar with the known benefits, limitations, and potential harms linked to breast cancer screening.
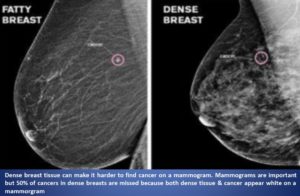
Limitations of mammogram: DID YOU KNOW MAMMOGRAM MAY MISS TUMOR ?
- Dense Breast: A false-negative mammogram looks normal even though Breast cancer is present. Women with dense breast have more false-negative results. Breast tissue is composed of milk glands, milk ducts and supportive tissue (dense breast tissue), and fatty tissue (non-dense breast tissue). Mammogram determines the ratio of non-dense tissue to dense tissue and assigns a level of breast density. Dense breast tissue makes it more difficult to interpret a mammogram, since cancer and dense breast tissue both appear white on a mammogram. On a mammogram, non-dense breast tissue appears dark and transparent. Dense breast tissue appears as a solid white area on a mammogram, which makes it difficult to see through. Supplemental tests for breast cancer screening with Dense Breast may include: 3-D mammogram breast tomosynthesis; Breast MRI; Breast ultrasound; Molecular breast imaging (MBI).
- A false-positive mammogram looks abnormal even though there is no cancer in the breast. Abnormal mammograms require unnecessary extra testing (diagnostic mammogram, ultrasound, sometimes MRI or even breast biopsy) to find out if the change is cancer
- Radiation exposure: Because mammograms are x-ray tests, they expose the breasts to radiation. The amount of radiation from each mammogram is low, but it can still add up over time.
Clinical Breast Exam: A clinical breast exam is an examination by a doctor or nurse, who uses his or her hands to feel for lumps or other changes.
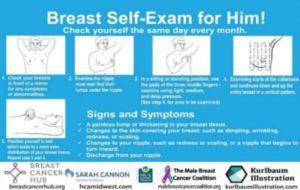
Breast Self-Exam from 17-18 years of age: Being familiar with how our breasts look and feel can help us notice symptoms such as painless or painful lumps, pain, or changes in size that may be of concern. These could include changes found during a Breast self-exam. We should report any changes that we notice to our doctor or health care provider. Please find below a protocol to do Breast self-exam for both women and men since Breast cancer rate in men is also increasing and most men with Breast cancer seem to have experiences of shock and subsequent embarrassment, battling the “stigma” of having a predominately woman’s disease.
 Breast Cancer Hub produced the Breast self-exam card in multiple languages for both women and men, in collaboration with Male Breast Cancer Coalition (www.malebreastcancercoalition.org), Sarah Cannon Cancer Institute & Kurlbaun Illustration, the authentic correct protocol to follow. Please download the card of your native language and perform the BSE. https://www.breastcancerhub.org/news-2/self-breast-exam-card.
Breast Cancer Hub produced the Breast self-exam card in multiple languages for both women and men, in collaboration with Male Breast Cancer Coalition (www.malebreastcancercoalition.org), Sarah Cannon Cancer Institute & Kurlbaun Illustration, the authentic correct protocol to follow. Please download the card of your native language and perform the BSE. https://www.breastcancerhub.org/news-2/self-breast-exam-card.
Embarrassment, Taboo, Ignorance:
In many parts of the developing world, in-spite of women doing so well in every sphere of their lives, even in educated and economically solvent segments, Breast cancer mortality is high due to lack of awareness and early detection screening. Breast cancer screening is a low priority and the knowledge of self- breast examination, clinical breast examination & other screening methods is very limited. Women & family members even hesitate to mention the word cancer in “Breast”. It’s the shyness & embarrassment society imposes. It’s the stigma, awkwardness and taboo of using the word “Breast”. Let’s strive together in our journey against Breast cancer by coming out of the stigma, awkwardness and taboo of using the word Breast! Let us help both women as well as men understand the importance of screening processes and translate the knowledge.
Also Read: “Shhhh….. Let’s not discuss,” writes Dr. Lopamudra Das Roy
**Dr. Lopamudra Das Roy (M.Sc, Ph.D, MBA) is the Founder and President, Breast Cancer Hub. Original Article -© 2020 Breast Cancer Hub, All Rights Reserved.




